Table of Contents
d. Minimally Invasive Glaucoma Surgery (MIGS)
Aging Eyes
As the body ages, vision may deteriorate, and eyeglasses may be needed. You may need to have brighter lights around the house to prevent accidents. You may also need to see your eye doctor more frequently. This is a normal part of aging, but the eyes can experience more severe problems that require surgery or prescription medications.
Age-related eye disorders like glaucoma and cataracts become more common as you age. Azopt (brinzolamide), Zymar Ophthalmic Solution or Lotemax (loteprednol)can be prescribed to improve these disorders. Aging eyes may also become more sensitive to heat and cold, becoming more prone to unpleasant dry eye symptoms. You may be prescribed Patanol (olopatadine) and Zaditor eye drops to relieve these symptoms and any other accompanying allergy symptoms.
Medications are helpful, but sometimes they are not effective enough to completely assist in severe forms of cataracts or glaucoma. In these instances, you may require surgery to improve your eyesight and quality of life. Read on to learn more about the treatment options available for age-related eye disorders. [1]
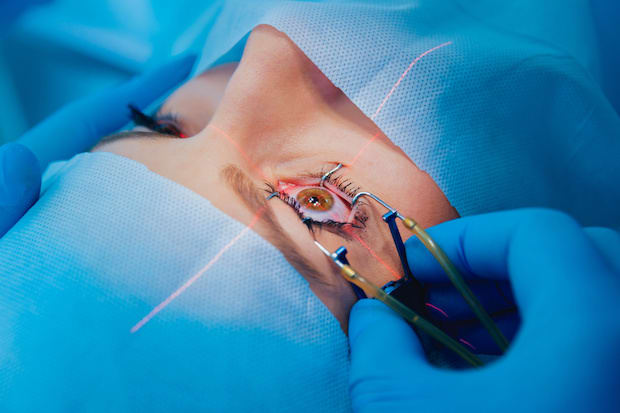
Glaucoma is an eye condition that targets and damages the optic nerve. High pressure in the eye can damage the optic nerve and lead to blindness, especially for those over 60. Glaucoma is a dangerous condition because it often has no symptoms or warning signs and may start off as slight vision loss. Your eye pressure is checked at every eye appointment to check for this condition. Vision typically cannot be regained or reversed if your optic nerve is damaged. Treatment aims to improve how fluid drains from the eye and decrease eye pressure. You will likely be prescribed prescription eye drops, oral medications, or undergo surgery in severe cases. [2] Carbonic anhydrase inhibitors: reduce the production of fluid in the eye. Azopt (brinzolamide) eye drops can be used twice a day (or as prescribed by your doctor) to help with glaucoma symptoms. Side effects can include metallic taste, frequent urination, and tingling of the fingers and toes. Beta-blockers: drugs like Betopic (betaxolol) can reduce the fluid in your eye and lower intraocular pressure. Side effects include slowed heart rate, lower blood pressure, and fatigue. Rho-kinase inhibitor: lowers fluid production by suppressing rho-kinase enzymes that are responsible for the fluid increase. Side effects of these drugs may include eye redness, eye discomfort, and deposits forming on the cornea. [2] The type of laser surgery you receive depends on the type of glaucoma and the severity of your condition. These lasers produce a beam of light that makes a small burn and open the eye tissue. For example, argon laser trabeculoplasty (ALT) is used for primary open-angle glaucoma. This involves a laser beam opening the eye's fluid channels to help the eye drain more efficiently. There are several laser treatments available, and other types include: Your eye will be numbed with medicine before the surgery, and your vision may be a bit blurry once the procedure is completed. Laser surgery is considered a fairly safe procedure, and people can typically resume daily activities the day after surgery. [3] A tube-shunt surgery can also reduce eye pressure. A tube-shunt surgery involves placing a flexible plastic tube with an attached silicone drainage pouch to the eye. This device assists in fluid drainage. This procedure is done for those with difficult cases of glaucoma. It is also common for those with diabetes-related eye pressure problems. Over half of tube-shunt surgeries are completely successful. [4] As its name suggests, this surgery is less invasive, not as risky as other methods, and requires less immediate postoperative care. The types of MIGS include trabecular surgery, suprachoroidal shunts, and microtrabeculectomies. These surgeries involve removing parts of the trabecular meshwork, which is essential in the eye's drainage function. Shunts may also be used to create a small opening to allow better fluid drainage. [5] Cataracts occur slowly and cloud the normally clear lens of the eye. Those with cataracts may feel like they are looking through a frosty or fogged-up window. Having cataracts can make it increasingly difficult to drive a car and read properly. Stronger lighting and eyeglasses can assist in the early stages of cataracts, but surgery may be necessary as it progresses. [6] Your doctor will determine when it is time to perform cataract surgery. You will likely undergo surgery if your cataracts begin affecting your everyday life and normal activities. Cataracts do not harm the eye, so there is no rush for surgery for some people. The surgery involves removing the clouded lens and replacing it with an artificial lens (intraocular lens). The new lens will remain a permanent part of the eye and improve your cloudy vision. This is generally an outpatient procedure, and a patient will not have to stay overnight at the hospital. A doctor will use a local anesthetic to numb the area around the eye. The patient remains awake during the procedure. You may have some discomfort a few days after the surgery, but this should subside within a few weeks. The only risks for cataract surgery include infection and bleeding. You will likely be prescribed Zymar Ophthalmic Solution or Lotemax (loteprednol) to use post-surgery to prevent any ocular inflammation or pain. In some rare cases, retinal detachment may occur. Talk to your doctor if your cataracts are disrupting your normal activities. [6] The content in this article is intended for informational purposes only. This website does not provide medical advice. In all circumstances, you should always seek the advice of your physician and/or other qualified health professionals(s) for drug, medical condition, or treatment advice. The content provided on this website is not a substitute for professional medical advice, diagnosis, or treatment.
Glaucoma Treatments
a. Medicated Eye Drops
b. Laser Therapy
c. Drainage Tubes
d. Minimally Invasive Glaucoma Surgery (MIGS)
Cataract Treatment
a. Cataract Surgery
