Table of Contents
I. What is Ulcerative Colitis?
III. Primary Sclerosing Cholangitis
IV. Lack of Growth and Development
What is Ulcerative Colitis?
Ulcerative colitis can be a painful condition with unpleasant symptoms like chronic diarrhea and abdominal pain. Ulcerative colitis is a type of bowel inflammation that occurs along with ulcers in the large intestine. Ulcers are little sores that form in the innermost lining when cells in the stomach lining die. These ulcers typically begin in the rectum and work their way up the digestive tract. Ulcers can lead to bleeding and a discharge of mucus and pus. This chronic inflammation can lead to the contents of the bowel to move rapidly and empty frequently. [1]
Ulcerative colitis can affect anyone, but the severity of symptoms can differ from person to person. UC symptoms can also change over time, so it is important to stay in contact with your healthcare provider to keep an eye on your condition. Common symptoms can include:
- Increased abdominal sounds
- Abdominal pain
- Bloody stools
- Weight loss
- Malnutrition
- Diarrhea
- Fever
The presence of blood and the frequency of diarrhea can lead to several complications. Dehydration and malnutrition are two common problems for those with UC. Still, it is important to get these symptoms under control with medications like Imuran (azathioprine), Asacol (mesalamine), and Neoral (cyclosporine). Long-term control medications are beneficial, but other conditions may begin to occur if you live with ulcerative colitis. [2]
Research has found that those with ulcerative colitis are at an increased risk of developing osteoporosis. Osteoporosis is a condition that typically affects postmenopausal women. The density of bone mass decreases as people age, increasing the risk of bone fractures. Several factors can result in osteoporosis, including ulcerative colitis. For many, dairy products are triggering to the intestines of UC sufferers. This can become problematic over time because bone health relies on the consumption of vitamin C, which is typically found in milk products. Calcium deficiencies can cause bones to weaken and increase your risk of osteoporosis. You may have to take dietary supplements to get all the vitamins and minerals you need. [3] Corticosteroid use with UC can also increase your risk of osteoporosis. Using corticosteroid medications can affect how your body absorbs vitamins that are integral to bone health. Corticosteroids are used as an anti-inflammatory medication to help with UC symptoms. These steroids can affect how the body uses vitamin D to build bones, resulting in bone loss and eventually, osteoporosis. [4] Primary sclerosing cholangitis (PSC) is a serious complication of ulcerative colitis. This complication can result in jaundice, liver failure, and, eventually, liver transplantation. Due to stomach inflammation and scarring, the bile ducts can become damaged and blocked. Bile is a digestive liquid made in the liver and can cause damage to other body systems. When the bile is blocked, it begins to accumulate and damage liver cells and eventually cause cirrhosis of the liver. PSC typically happens slowly over time. [5] PSC can be difficult to diagnose because it usually does not have many symptoms. You may be experiencing your normal UC symptoms and not realize that you are also suffering from PSC. Symptoms of PSC can include: For most people, PSC does not become severe until 10-15 years after the initial diagnosis. Unfortunately, there are no specific treatments for this condition, but liver transplants may be required if it becomes severe. [3] If someone is diagnosed with ulcerative colitis early in life, it can significantly impact a person’s physical growth. In some cases, UC can delay puberty. If you have a child affected by UC, you should frequently take your child for height and weight check-ups at the doctor. This can help the doctor keep track of your child’s growth and determine if their UC is affecting their development. It is recommended to have these check-ups every 3-12 months. [3] A person’s growth can be affected due to malnutrition. With UC, the bowels move food quickly through the intestines, making it difficult for the body to absorb vitamins and minerals. Severe diarrhea associated with UC can cause dehydration, which results in your body lacking the proper fluids, nutrients, and electrolytes. You may be experiencing malnutrition if you have the following symptoms: This serious complication can also lead to painful symptoms. Toxic megacolon is a rare condition that occurs when UC inflammation leads to gas becoming trapped in the colon. This leads to an enlarged and swollen colon. Gas in the colon is a serious problem and can lead to a rupture of the colon. If the contents of the colon spill out into the rest of the body, septicemia (an infection of the blood) can occur. Septicemia can result in death if it’s not detected early. You may be experiencing toxic megacolon if: If you catch these symptoms in time, toxic megacolon can be treated with antibiotics and steroids. Surgery may be needed to reduce colon pressure in more severe cases. If you manage to control your ulcerative colitis symptoms successfully, it is unlikely you will experience toxic megacolon. [3] Those with ulcerative colitis are at an increased risk of developing bowel cancer. Because of this, it is essential to pay attention to any changes in your symptoms and have frequent doctor check-ups. Bowel cancer involves cancer of the colon, rectum, or bowel. [3] Bowel cancer is a more common type of cancer and is typically diagnosed in adults over 60 years old. Symptoms of bowel cancer are a bit more severe than UC, but not altogether dissimilar. The three main symptoms include: Typically, these symptoms do not result in bowel cancer, but you should seek a doctor's advice if you have UC and the above symptoms. Your doctor will typically perform a colonoscopy to look for signs of cancer in your intestines. This involves inserting a flexible tube containing a camera into the rectum. Depending on your risk of bowel cancer, you may undergo a colonoscopy every one to five years. [7] The content in this article is intended for informational purposes only. This website does not provide medical advice. In all circumstances, you should always seek the advice of your physician and/or other qualified health professionals(s) for drug, medical condition, or treatment advice. The content provided on this website is not a substitute for professional medical advice, diagnosis or treatment.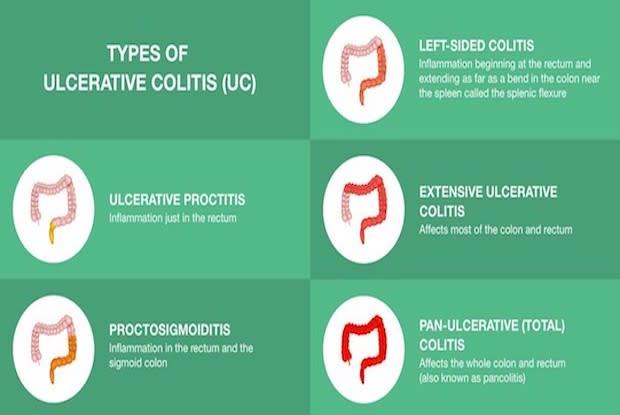
Osteoporosis
Primary Sclerosing Cholangitis
Lack of Growth and Development
Toxic Megacolon

Bowel Cancer
