Table of Contents
II. How do Insulin and Glucose Work?
III. Type 1 vs. Type 2 Diabetes
IV. What are the Symptoms of Type 2 Diabetes?
VI. Medications for Type 2 Diabetes
What is Type 2 Diabetes?
Type 2 diabetes is an increasingly common condition in the United States. There are over 34 million Americans with diabetes, and around 90 to 95 percent of them have type 2. This condition occurs when there is a problem with how the body uses and regulates sugar (glucose). [1]
There is no exact reason behind type 2, but it is thought that being overweight and inactive are two contributing factors. Type 2 usually occurs slowly over time and happens when cells in the muscle, fat, and liver become resistant to insulin. These cells do not consume enough sugar to fuel the body, so excess sugar is floating around the bloodstream. The other problem has to do with the pancreas. The pancreas is unable to produce enough insulin to manage blood sugar levels in the body.

This disease can be reversed in some patients, but people often have to make several purposeful changes in their lifestyle to regulate their blood sugar. In the meantime, your doctor may prescribe an insulin treatment along with medications like Rybelsus, Januvia, or Jardiance to help you deal with diabetes. Learn more about the symptoms of type 2 diabetes below. [2]
How do Insulin and Glucose Work?
To fully understand type 2 diabetes, the role of glucose and insulin must be addressed. As mentioned briefly above, glucose is the main energy source for cells that make up muscles and bodily tissues. When food is broken down, the glucose within it enters the cells with insulin. Once your body uses all the glucose it needs, it stores the excess in the liver to be used later.
Insulin and glucose work in tandem with each other to keep the body nourished. Insulin regulates how the body uses glucose by:
- Triggering the pancreas to secrete insulin
- Enabling sugar to enter the cells
- Telling the pancreas to release less insulin
Type 2 diabetes occurs when these processes are not working properly. If your blood sugar spikes and dips for a long period, the cells may become damaged and the insulin-producing beta cells in the pancreas release more insulin, causing type 2 diabetes. [2]
Type 1 vs. Type 2 Diabetes
Both types of diabetes are due to unregulated glucose levels. These conditions are chronic, but they do have significant differences. In type 1 diabetes, the body does not produce insulin, while those with type 2 do not respond as well to insulin as they should. People with type 2 are more likely to develop it after 45, which differs greatly from type 1. Type 1 was referred to as juvenile diabetes because it is often diagnosed in childhood or adolescence.
Type 1 occurs due to a malfunction in the immune system. The body attacks itself and destroys insulin-producing beta cells in the pancreas. The body cannot produce insulin once these cells are destroyed. Insulin therapy is not always necessary for type 2 diabetes. [3]
What are the Symptoms of Type 2 Diabetes?
Around one in four people with type 2 are unaware they have the condition. Symptoms usually come on slowly, so you may not notice any changes at first, or you may grow used to them. But if any of the following symptoms strike you as abnormal, you should seek the help of your doctor.
- Increased hunger
- Increased thirst
- Increased urination
- Fatigue
- Blurry vision
- Loss of consciousness
- Slow-healing sores
- Red, swollen, tender gums [4]
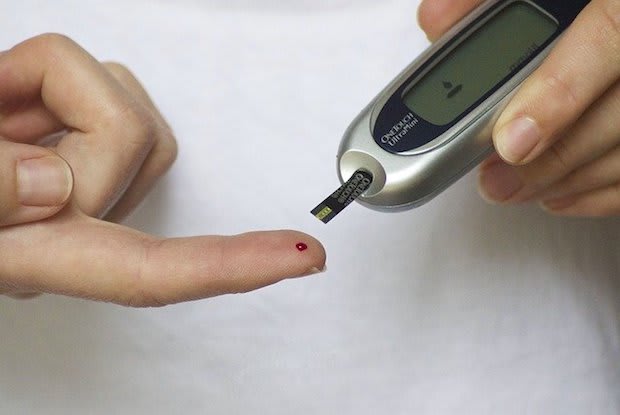
Diagnosing Type 2 Diabetes
An A1C (glycated hemoglobin) test is usually the first test given to diagnose type 2 diabetes. This test measures your average blood sugar level for the previous two to three months. You may also take a fasting blood sugar test, which is taken after an overnight fast.
In many cases, your doctor will subject you to a diabetes screening at your yearly physical. These screenings are mostly for people over 45. Still, you may be screened for diabetes at a younger age if you are overweight or obese, had gestational diabetes, or have a family history of type 2 diabetes. [2]

Medications for Type 2 Diabetes
Treating type 2 often requires a multi-faceted approach. Depending on the cause of your diabetes, you will likely have to alter your diet to include more healthy foods and participate in more physical activity.
Along with these lifestyle changes, you should follow your doctor’s instructions when taking type 2 diabetes medications. Drugs such as Rybelsus are highly effective, but it is important to take Rybelsus properly to maximize safety and efficacy.
Jardiance is another popular treatment used to manage type 2 diabetes. It works by improving glycemic control and lowering your blood sugar levels. With the help of prescription medication, you can minimize your symptoms and how much diabetes affects your life.
There are many more kinds of type 2 diabetes medications available, such as Januvia, Tradjenta, and Ozempic. With many choices, it is important to work with your doctor to determine the right treatment for you. Type 2 diabetes may change your life in many ways, but it is possible to live a full life by taking the right steps to manage your symptoms.
The content in this article is intended for informational purposes only. This website does not provide medical advice. In all circumstances, you should always seek the advice of your physician and/or other qualified health professionals(s) for drug, medical condition, or treatment advice. The content provided on this website is not a substitute for professional medical advice, diagnosis, or treatment.
