Table of Contents
I. Crohn’s Disease vs. Ulcerative Colitis
II. Diagnosing Inflammatory Bowel Diseases
IV. Complications of UC and Crohn’s Disease
Crohn’s Disease vs. Ulcerative Colitis
Both Crohn’s and ulcerative colitis (UC) are inflammatory diseases that are caused by an abnormal immune response in the body. Ulcerative colitis differs from Crohn’s because UC only affects the large intestine. Crohn’s affects both the colon and small intestine, and can in fact affect the entire GI tract. Crohn’s locations could include the mouth and anus, and even in the genital area. Both of these conditions are inflammatory bowel diseases (IBD). Signs of Crohn’s and ulcerative colitis are often similar and typically involve:
- Weight loss
- Cramping
- Fatigue
- Severe diarrhea
- Abdominal pain
- Malnutrition [1]
Ulcerative colitis (UC) can be more severe than Crohn’s due to the presence of ulcers. The exact cause of UC is unknown, but it is more common than Crohn’s. In the case of UC, the inflammation starts at the anus and extends into the large intestine. Ulcers are sores that can form in the lining of the stomach and can lead to severe complications like stomach bleeding and malnutrition.
Both of these conditions affect both men and women equally. There is no exact cause for either bowel disease, so it is believed to be a combination of environmental and genetic factors. Around 10 percent of inflammatory bowel disease exhibit features of both Crohn’s and UC equally. [2] This is known as indeterminate colitis. These two conditions are so similar that they are often treated with the same medications. Mesalamine is one such drug that can help with symptoms of these two bowel diseases. If your doctor has prescribed you this medication you can buy mesalamine online through RxConnected to save money. Read on to learn more about Crohn’s, UC, and mesalamine as a treatment. [2]
Get savings updates for Mesalamine
Diagnosing Inflammatory Bowel Diseases
There are several tests that your doctor may perform to determine the cause of your gastrointestinal issues. Many conditions can cause abdominal pain and diarrhea, so blood tests and other procedures will likely be recommended. If you want to learn more about gastrointestinal disorders, visit RxConnected’s blog to learn more. Some tests can include:
Blood test: A blood test may be taken to rule out anemia (lack of red blood cells) or any other sort of infection. Infections also cause inflammation, so a blood test may help single out the cause of any pain or redness in the abdomen.
Fecal occult blood test: A stool sample can tell your doctor a lot about the state of your intestines. Your doctor will examine your stool sample for signs of blood, which signifies a bowel problem like Crohn’s or UC.
Colonoscopy: Colonoscopies are useful because they give your doctor a full view of the entire colon. This procedure involves inserting a flexible, lighted tube into the rectum. The end of this tube is equipped with a camera so your doctor can view the stomach lining. If clusters of inflammatory cells (granulomas) are present, you likely have Crohn’s. [1]
Capsule endoscopy: This test involves swallowing a capsule equipped with a tiny camera. This camera will then take pictures of your small intestine, which can be downloaded to a computer and examined. This test is most successful in diagnosing Crohn’s.
X-ray and MRI: X-rays are used if you are suffering from severe symptoms. A perforated colon or other abnormality can be seen in an x-ray. Magnetic resonance imaging (MRI) can also be used to create detailed images of organs and tissues. MRIs are useful in evaluating the small intestine in the case of Crohn’s. [3]
What Does Mesalamine Do?
Mesalamine was approved for the treatment of ulcerative colitis and Crohn’s disease over 30 years ago. The main function of this medication is to reduce inflammation in the colon. Many substances within the body are responsible for inflammation. Prostaglandins are responsible for inflammation in the colon and produce the enzymes, cyclooxygenase, and lipoxygenase. Bowel problems occur when these two enzymes are overactive. Mesalamine works to reduce the presence of these enzymes in the body and improve bowel inflammation symptoms. [4]
This medication can come in several different forms and dosages, depending on the severity of your bowel problems. Mesalamine belongs to a class of drugs known as aminosalicylates. Aminosalicylates are responsible for reducing inflammation in the lining of the intestines. RxConnected has many types of mesalamine, and your doctor will prescribe the right one for you. RxConnected carries Asacol, Pentasa, Lialda, and the Canasa suppository. If you are taking an oral version of this drug, it is essential to swallow it whole. Do not crush or chew the tablet or capsule because it can disrupt its release into the colon. If you cannot swallow tablets whole, you can break them open and sprinkle the contents on applesauce or yogurt and then take it. It is important to keep a drug schedule and take mesalamine at the same time(s) every day. [5] It may take some time to get the full effects of a mesalamine treatment. Common side effects of this drug include headache, flatulence, itching, and hair loss. Contact your doctor if you experience the following severe side effects of mesalamine: Experiencing inflammatory bowel disease can put you at risk for developing complications and other painful conditions. Medications and colon surgery can help relieve abdominal pain and inflammation, but bowel disease’s long-term side effects may take its toll on the body. The following may occur as a result of UC or Crohn’s: Fistulas: Fistulas are common in those who live with Crohn’s disease. Fistulas are tunnel-like structures that form and connect the bowel parts to other organs, including the bladder, vagina, or skin. In the case of Crohn’s, the fistula usually forms in the tissue surrounding the anus. Around one in three people with Crohn’s will develop a fistula. [6] Bowel Cancer: Bowel is one of the most common types of cancers in adults. Your risk for bowel cancer depends on how long you’ve had Crohn’s or UC, how much of your colon is affected, and the severity of your bowel inflammation. Bowel cancer usually begins with polyps (growths) that may or may not become cancerous. [7] Intestinal Strictures: Intestinal strictures occur when the intestines narrow and make it challenging for food to pass properly. They can be mild or severe and can lead to complete blockages, which can lead to malnutrition. If fluid or food cannot pass through the intestines, then the body cannot receive any nutrients. If a stricture becomes severe, emergency surgery is required. [8] The content in this article is intended for informational purposes only. This website does not provide medical advice. In all circumstances, you should always seek the advice of your physician and/or other qualified health professionals(s) for drug, medical condition, or treatment advice. The content provided on this website is not a substitute for professional medical advice, diagnosis or treatment.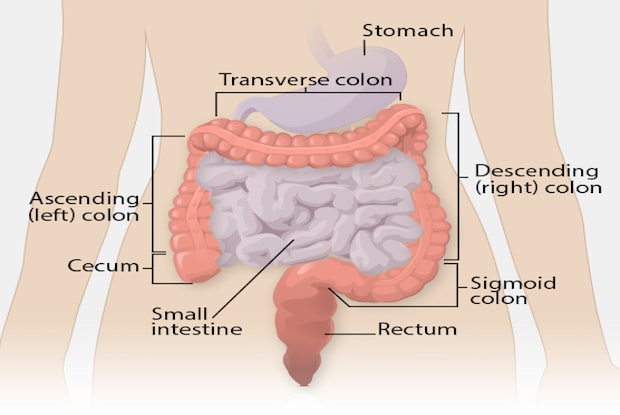
a. Side Effects of Mesalamine
Complications of UC and Crohn’s Disease