Table of Contents
I. What is Ulcerative Colitis?
III. Colitis vs. Ulcerative Colitis
IV. Types of Ulcerative Colitis
V. Triggers for Ulcerative Colitis
What is Ulcerative Colitis?
Ulcerative colitis is an inflammatory bowel disease that affects over 750,000 people in North America. [1] This chronic disorder has no known cause. Ulcerative colitis can occur in flare-ups throughout a person’s life. Ulcerative colitis (UC) occurs when the inner surface of the rectum and colon become inflamed and can cause irritation, inflammation, and ulcers in the large intestine lining. [1]
Ulcerative colitis is an autoimmune disease that occurs when the body mistakenly attacks itself. The body begins to attack the good gut bacteria, food, as well as cells in the large intestine. White blood cells attack these body processes and lead to inflammation of the colon lining. UC can be difficult to diagnose because many stomach disorders have similar symptoms. Read on to learn more about signs and symptoms of ulcerative colitis, as well as treatment medications like Imuran (azathioprine), Asacol (mesalamine), and Neoral (cyclosporine). [2]
There are several uncomfortable symptoms of ulcerative colitis. The main symptom is bloody diarrhea, but the ulcers can lead to other adverse symptoms. Ulcers are sores that occur in the lining of the stomach due to inflammation. Ulcers can also lead to the presence of pus in stools. More symptoms can include: Symptoms of ulcerative colitis can occur in bursts and may not occur for several months or years. It is essential to get these symptoms under control because excessive bloody diarrhea can cause dehydration if left untreated. [2] Ulcerative colitis can happen to anyone. Doctors and researchers have not pinpointed an exact cause so that several factors can result in this autoimmune disease. Genetics play a major role, and this condition sometimes runs in families. Your risk of developing ulcerative colitis is 30 percent higher if you have a close family member with this condition. Those between the ages of 15 and 30 and those older 60 are most at risk for UC. People who are of Ashkenazi Jewish descent are at the highest risk of developing ulcerative colitis. [2] Colitis is the more general type of inflammation in the lining of the colon. This disorder also causes abdominal pain, diarrhea, and bloody stools. Patients may experience colitis and not ulcerative colitis. The difference between the two conditions depends on the formation of ulcers in the colon. A doctor can determine if ulcers are present through a colonoscopy. A colonoscopy is a wand with a camera at the end. It is inserted into the rectum and up into the colon. If the camera detects ulcers, the doctor may take a tissue sample from the colon to determine the cause. [3] There are several different types of colitis. Doctors typically classify the type of colitis by its location in the body. The types of ulcerative colitis can include: Pancolitis (universal colitis): This type affects the entire colon and can cause periods of severe bloody diarrhea, cramps, fatigue, and weight loss. Ulcerative proctitis: Ulcerative proctitis is the mildest form of ulcerative colitis. It is confined to the area closest to the anus, and rectal bleeding is the first sign of this condition. Acute severe ulcerative colitis: This is the rarest form of colitis and affects the entire colon. The symptoms often include severe pain, bleeding, fever, profuse diarrhea, and an inability to eat. Left-sided colitis: This type involves inflammation that extends from the rectum up through the sigmoid and descending colon. The symptoms are similar to the other types, but the pain occurs on the left side and may cause unintended weight loss. Proctosigmoiditis: This type involves inflammation of the rectum and the lower end of the colon. Proctosigmoiditis can result in an inability to move bowels, cramps, and bloody diarrhea. [4] Because the cause of ulcerative colitis is unknown, it can be helpful to avoid any triggering foods or substances. Ulcerative colitis is not caused by one singular food or beverage, but some can make your symptoms worse. It is good to keep a food journal to track what activities and foods can trigger symptoms of diarrhea, cramps, and trouble defecating. Some foods that may cause flare-ups can include: Whole-grain foods: Whole grains have fibrous germ, endosperm, and bran that may irritate ulcerative colitis. You should avoid brown rice, quinoa, buckwheat, oats, and wild rice. Nuts and seeds: Nuts can be very hard to digest. A person with UC should avoid nuts in cooked foods as well as nut-based flours. You may want to avoid macadamia nuts, peanuts, cashews, walnuts, hazelnuts, pecans, almonds, and pistachios. Seeds are also insoluble fiber. Avoid sesame seeds, pine nuts, pumpkin seeds, flax seeds, and millet. Fibrous fruits and vegetables: The fiber in fruits and uncooked vegetables can be difficult to digest. Typically they are easier to digest if they have no seeds, are cooked, and peeled. It is important to avoid dried, raw, and seedy fruits like berries. Dried beans and lentils: Legumes and high protein foods have indigestible sugars within them. They also can cause gas, which further irritates UC. Those experiencing a flare-up may want to avoid all beans, adzuki beans, soy nuts, edamame, and soybeans.[5] There are several ways to diagnose ulcerative colitis. It is important to tell your doctor all your symptoms so they can rule out any other possible causes of your stomach discomfort. Your doctor may order a blood test to check for anemia, which occurs when there are not enough blood cells to carry oxygen. A stool sample is another common way to check for UC. A stool sample can also rule out any other complications like bacterial infections, viruses, or parasites. As mentioned earlier, colonoscopies allow the doctor to get a good view of the colon and determine any abnormalities. A tissue sample from a colonoscopy can also help confirm UC. A flexible sigmoidoscopy is a similar device used to detect inflammation. For this procedure, the doctor will insert a lighted tube into the rectum to examine the lower portion of the colon. This lighted tube can see if the colon is inflamed, which is a sign of UC. [4] In general, drug therapy or surgery is needed to treat UC properly. Your treatment will depend on the severity of your UC symptoms and their impact on your everyday life. For moderate to severe ulcerative colitis, corticosteroids may be prescribed to reduce inflammation. In the case of more severe UC, your doctor may prescribe immunomodulator drugs. These drugs also reduce inflammation by suppressing the immune system and preventing further inflammation. Imuran (azathioprine) is one example of an immunomodulator. Neoral (cyclosporine) can also be used for UC. It is typically used for organ transplant patients, but can also reduce inflammation in colitis patients. [6] Asacol (mesalamine) can also be used to treat certain bowel diseases. This drug is an aminosalicylate, which works to decrease swelling in the colon. It can also reduce symptoms of diarrhea, rectal bleeding, and stomach pain. [7] If UC cannot be controlled with medications, surgery can be a successful treatment method. One extreme tactic involves removing your entire colon and rectum. A less intensive surgery involves the surgical creation of a pouch at the end of the intestine. This pouch is attached directly to the anus and allows you to expel waste normally. [4] The content in this article is intended for informational purposes only. This website does not provide medical advice. In all circumstances, you should always seek the advice of your physician and/or other qualified health professionals(s) for drug, medical condition, or treatment advice. The content provided on this website is not a substitute for professional medical advice, diagnosis or treatment.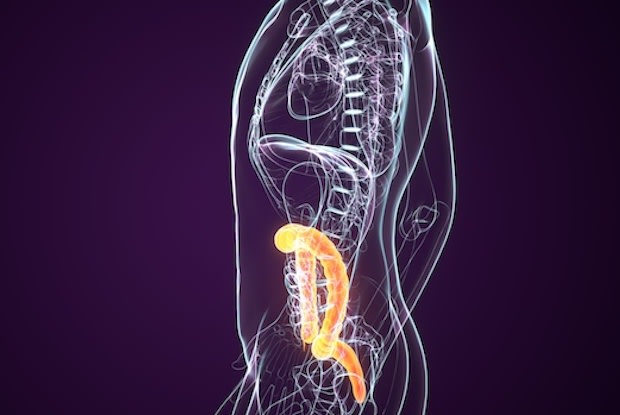
Symptoms

a. Risk Factors
Colitis vs. Ulcerative Colitis
Types of Ulcerative Colitis
Triggers for Ulcerative Colitis

Diagnosis
Treatment
